2024 has been a year of change. A tough year for so many, with no let up in the cost-of-living crisis for our clients and for so many of us across the country.
What's more, so many of us as individuals, communities and across our sector, are dealing with increased pressures of the continuing housing crisis, the rise of hate crime and financial insecurity, among other things.
As a result, the mental health, social care and housing systems are under severe pressure once again.
Changing times
Change came at a national level in the summer with the arrival of a new Government; mission-led and determined to do things differently.
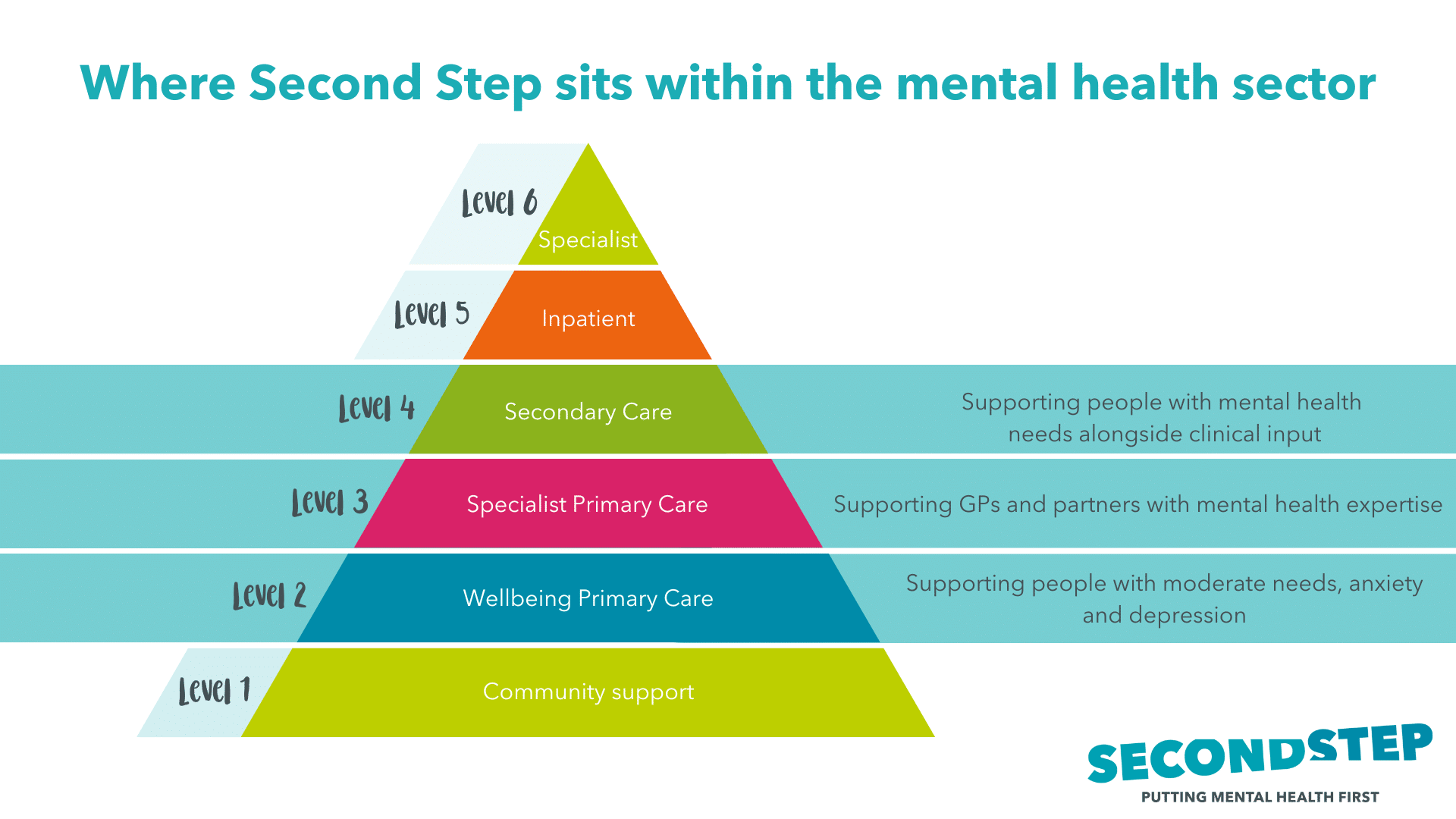
For the health and social care sectors, which account for around 20% of public expenditure, this heralds a rebalancing and a promise of a policy shift away from acute hospital care towards primary and community care - and a promised focus on earlier intervention and improved use of digital across the system.
At Second Step we support people experiencing moderate to severe mental health problems in their communities. We play a pivotal role, alongside our public sector and voluntary sector partners, to strengthen and develop the support offered in this space; while understanding the pressures on the wider system.
In this our Impact Report of 2024, we have chosen to highlight some key statistics together with some inspiring stories - to give you a flavour of the work we do and its impact on individuals and communities.
Supporting people at the right time
In this report, we demonstrate the essential work we do on prevention and early intervention. We support people in their homes and communities to find the hope and courage they need to change their lives for the better.
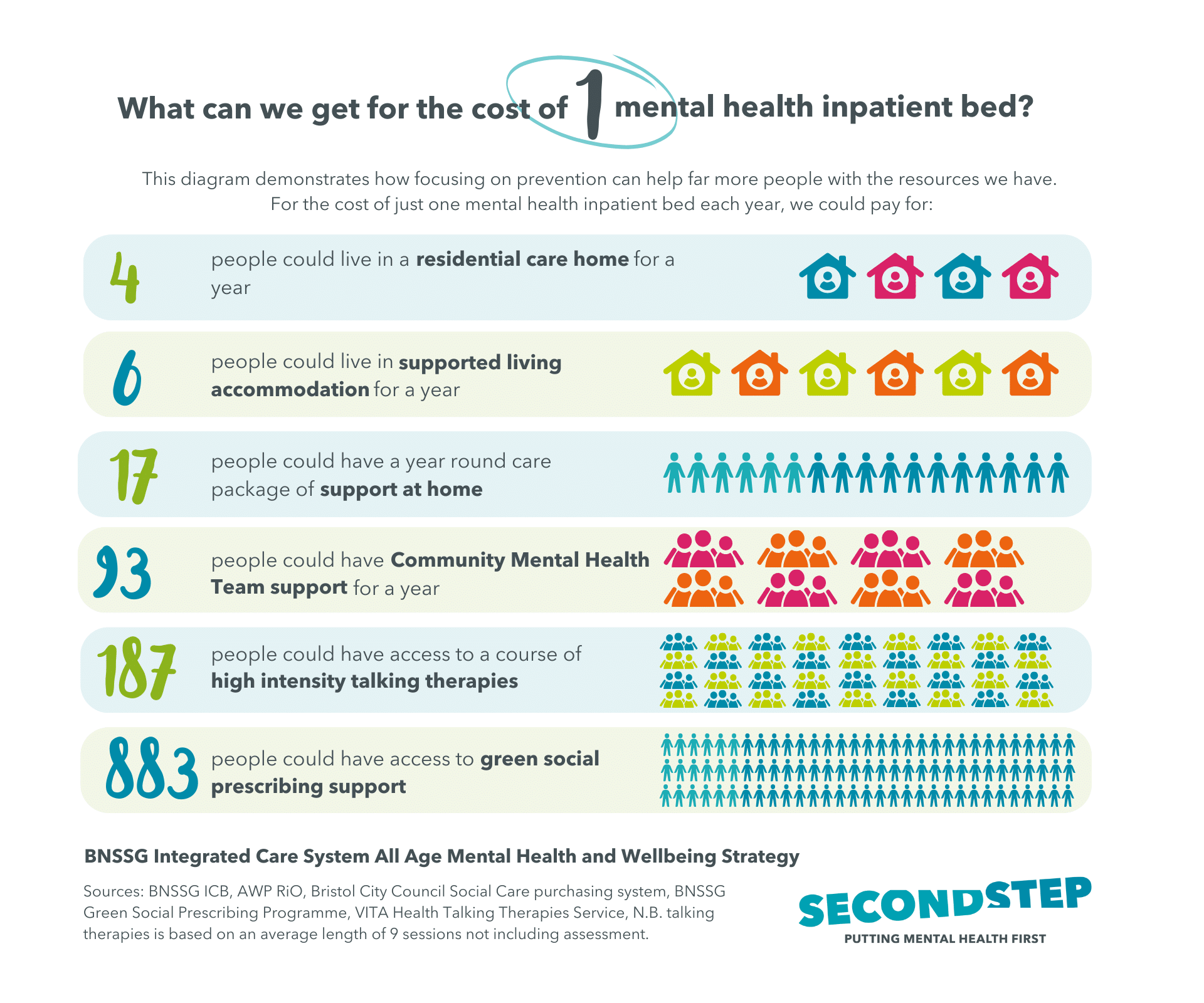
The statistics below are from the Bristol, North Somerset and South Gloucestershire (BNSSG) Integrated Care System. They commission many of Second Step's services and oversee the commissioning and delivery of all NHS mental health services in the region.
The graphic below demonstrates how effective it can be to focus on early intervention and prevention where we can.
Our skilled staff team uses a trauma-informed approach, helping clients build resilience and turn their lives around. We don't give up on anyone, even when they feel hopeless - as you can see from Rachel's story.
Our recovery navigators work as part of the new community mental health MINT teams, freeing up GPs and triage services. The Community Rehabilitation teams help keep people out of hospital, and our out-of-area team bring people back to their families and communities. We play a key role in preventing issues from worsening, understanding the social factors impacting lives, and supporting long-term solutions.
Looking back at our work this year, we're reminded of the power of prevention and the positive impact we've made on people's lives together with our public sector and voluntary sector partners.

Aileen Edwards
Chief Executive

Kelvin Blake
Chair of the Board
"I'm happy to be alive and be here today, because of you guys"
Drew's story
Drew's story highlights the power of early intervention, finding ways to support people before they feel like they have nowhere to turn. It seemed the perfect way to introduce the theme of our Impact Report for 2024: the Power of Prevention.
When Drew first made contact with our men's suicide prevention project, Hope, he was struggling to see a way forward. He shared with us how he felt during that time: "I needed help so badly. No one was there. No one was here to hear me. I needed someone. I couldn't talk to anyone."
For many men, societal pressures to 'tough it out' can make it harder to seek support. Yet, it’s a misconception that men don’t want help.
For Drew, meeting Ezra, his Hope Project worker, was a turning point. The strength of their bond became the foundation for Drew to rebuild his confidence, rediscover his passions, and make positive changes in his life. The trust and understanding they shared gave Drew not just the courage to keep going, but the belief that a fulfilling life, full of hope and purpose, was within his reach.
This is the power of prevention.


Drew’s story reminds me that, when meeting any new client, it is so important to be human and to support them in feeling safe. Once they feel safe, they feel able to talk openly and often – we may be the first people they’ve ever felt able to do that with.
Drew has been on a huge journey, from near homelessness to independent living, and he has worked extraordinarily hard to achieve all his goals. His passion for life, his sense of humour, his friendliness, compassion for others, his never-ending dedication to make things better, has been inspirational to me and to others."
– Ezra reflects on her work with Drew and other men through the Hope Project.
Our approach
Internally our focus is four-fold as laid out in our Strategic Plan to:

Build an inclusive culture with a continued priority to root out racism across the organisation, especially important in the context of the 2024 summer riots.

Embed our psychological, adversity and trauma-informed approach in all our interactions and all the work we do, learning together with our partners.
Value lived experience at every opportunity to ensure our clients’ voices and views are heard and acted upon with a new coproduction strategy due to go live in 2025 to ensure we hear more deeply from our clients, and improve services.
Create an enabling organisation where everyone contributes as fully as they can to work at the top of their skill set. In this way we improve our services and support the system as a whole to improve too.
Externally we are taking this inclusive, enabling and trauma-informed approach to the work we’re doing with our clients, to support the partnerships we’ve built with organisations across the system and to help positively change the system as a whole.
Our partnerships
We build partnerships positively and intentionally across the mental health and social care system, recognising the importance of our value of succeeding together.
In Somerset we’re a proud partner of the Open Mental Health alliance working closely with other VCSE organisations and the NHS to ensure people can access the mental health care they need close to where they live.
In Bristol, North Somerset and South Gloucestershire we formed the VCSE Mental Health Alliance with like-minded organisations to help ensure our voice is heard and influence felt across the health and social care sectors in our region.
Also in Bristol we work with partners from across the city, including the City Council, to run Changing Futures. A system change programme, it supports people facing multiple disadvantage, and is part of a national initiative funded by Government and the Community Fund.
In late 2024 we won the commission to provide community mental health services across Bath and North East Somerset, Swindon and Wiltshire as part of the newly-formed Mental Health and Wellbeing Partnership.

Our five areas of work
In this Impact Report, we look at the work we're doing across the South West region. These are some examples of our work in five different key areas:
- Suicide prevention & crisis services – the Hope Project and the Sanctuary in Bristol, Safe Haven in North Somerset and Crisis Safe Space in Somerset
- Community mental health teams the MINT teams across BNSSG, Recovery Bristol Partnership in Bristol and wellbeing and recovery services as part of Open Mental Health in Somerset
- Wellbeing Colleges across Bristol, North Somerset and South Gloucestershire
- Homelessness & complex needs services working with people facing multiple disadvantage including High Needs Floating Support’s out of hospital work, the Link Team and Changing Futures in Bristol and Step Together and Step Down services in Somerset
- Community Rehabilitation teams, including our out of area work in Bristol, and Somerset

Hope Project
(Source: Hope Project data 2024)
Our innovative and evidence-driven suicide prevention project, Hope, provides short-term emotional and practical support for men aged 30-64, specifically those who are in psychological distress as a result of their finances, housing or employment. Nationally, according to the most recent statistics from 2022, around three-quarters of suicides registered were men, accounting for 74% of total suicides.
Our experienced suicide prevention workers work with men across Bristol, North Somerset and South Gloucestershire over a twelve-week period, and focus on helping men who aren’t currently using mental health services. We know that 62% of all suicides are by people who aren’t known or connected to any services.
Drew's story
When Drew first came to the Hope Project, he was at breaking point:

I lost myself, I lost everything. I felt I was in a different world and couldn’t control my emotions. I felt nothing was in my control."
He'd been the target of bullying his whole life, he was about to become homeless, and he didn't have much faith in services - he felt they couldn't see past his disabilities. He'd been let down too many times before and was considering suicide.
Then Drew met Ezra through our Hope Project. Ezra supported Drew to navigate many of the practical challenges he was struggling with, including securing emergency housing, then securing his own flat, and accessing benefits. Ezra also provided emotional support, such as working on mindfulness exercises together, and accompanying Drew to start going out in busy public spaces which he found too anxiety-inducing before.

Ezra showed me how to build back up and be confident again. She made me feel safe and literally gave me back my life. No other support system has been like it, here I’ve found my confidence again. She’s inspired me to be the person I want to be.”

Another important way Ezra supported Drew was to share in his interests and give him a space where he could express himself and feel pride about the things in his life that he enjoys. Ezra says:

I have had many men tell me that interests like gaming, films, YouTube, music, are their saving grace. They take them somewhere ‘other than’ where they are most of the time, somewhere that’s safe... When supporting men’s mental health and wellbeing, it is incredibly important to hear about their interests, to show interest and give them a space where they can talk about this."
Drew now feels positive and excited about the future. He runs his own businesses, runs a YouTube channel related to his interests, and has made many new friends. Drew also wants to start mental health volunteering with Second Step so he can share his lived experience to help others going through similar things.
He was able to access support at a time when he felt most vulnerable and Ezra's empathetic and trauma-informed approach meant she recognised how Drew's past trauma was intensifying the challenges he faced. With Ezra's support, those challenges were difficult, but not insurmountable, allowing Drew to find hope and courage to keeping moving forward.
> Crisis services & suicide prevention support
The Sanctuary
The Sanctuary, located at Gloucester House on the grounds of Southmead Hospital in Bristol, provides a safe space for people in acute emotional distress.
Open from Thursday to Monday, 6pm to midnight, the service extended to seven nights a week from January 2024 to January 2025, thanks to additional funding.
The Sanctuary supports around 125 people monthly through one-on-one psychosocial interventions and de-escalation techniques. We also refer clients to specialist services like drug and alcohol support, debt advice, and housing expertise.
From January to June 2024, 57 different services referred people to the Sanctuary. These organisations included 111, 999, Accident & Emergency, Urgent Assessment Centre, Street Triage, AWP response line, Crisis Line, job centres, the Department of Work and Pensions, social services, SARI, Refugee Rights, and the police.
This diverse referral network highlights the Sanctuary's role in preventing crises by equipping clients with tools like breathing techniques, the five ways to wellbeing, and helping them build awareness of their triggers and reactions.
(Source: Sanctuary data 2024)
Lisa's story
Lisa* called The Sanctuary after experiencing intrusive thoughts following a change in her antipsychotic medication. She was worried the medication wasn’t working and she was scared she was about to become unwell. She told us she was experiencing critical and negative voices that seemed to come from outside her head. She said the voices were her thoughts and was challenging them, but she was also starting to feel overwhelmed.
We listened to Lisa offering reassurance and validating her feelings throughout. She told us she had found groups helpful in the past and we suggested the Wellbeing College and also women’s mental health organisation Missing Link as places she could go for support. Lisa left the call calmer and with positive options of what next steps to take.
*not her real name
> Crisis services & suicide prevention support
Crisis Safe Space
"There has been a welcome downward trend in A&E admissions for mental health patients thanks in part to the work of Open Mental Health."
(Source: Somerset Integrated Care Board)
Crisis Safe Space provides out-of-hours support for Somerset residents, aged 18 or over, who are in emotional or psychological distress. We work in partnership with Mind in Somerset. The service offers both intervention to individuals who have reached crisis point, and a prevention service to those who might otherwise reach crisis point without appropriate support, with proactive aftercare and support where required.
The ultimate aim of the service is to support individuals with their mental health crises and enable them to manage them through planning, grounding techniques, coping mechanisms, and identification of ongoing support.
In the last year we have held 3111 appointments. Of these 215 people told us they would have tried to end their life if they hadn’t had the support of our service. 376 people said they would have used A&E instead, if we’d not been there as an option.
By providing a safe space for people to go to in crisis we are demonstrably saving lives – and also taking the pressure off our busy A&Es.

It’s been weekly sessions with a warm and compassionate worker who quickly formed an understanding of my issues. They have helped me find acceptance of my current life and hope for the future" – Crisis Safe Space client
MINT Teams in BNSSG
New mental health hubs or MINT (Mental health Integrated Network Teams) teams have been set up in Bristol, North Somerset, and South Gloucestershire (BNSSG) as part of the NHS’s plan to introduce more integrated community mental health services. MINT teams aim to provide integrated, high-quality, and personalised care closer to home.
MINT teams are multi-professional and collaborative and build a network of support for every individual. There are six place-based hubs, one for each locality area across BNSSG, ensuring that people get the right support at the right time. The teams are set up to consider the wider determinants of health such as housing, employment and financial health which affect us all.
Our recovery navigators play a crucial role in the core MINT teams. They engage in support conversations with clients to understand what matters to them and coproduce a personalised wellbeing plan. They provide brief clinical and psycho-social interventions and help people access further support in the community as part of their package of care.
By providing timely and appropriate support, recovery navigators help reduce the need for more intensive and costly interventions, thereby saving the health care system money.
The video clip below gives an overview of the MINT teams' work across BNSSG. Thank you to our partners at AWP for sharing this video.
> Community mental health hubs in Bristol, North Somerset and South Gloucestershire (BNSSG) and Somerset
Community mental health support in Somerset
Our recovery and wellbeing workers support people on their journeys towards improved mental health, wellbeing, and recovery.
We provide high-quality support for people with moderate to serious mental health needs, primarily on a one-on-one basis across the Sedgemoor locality in Somerset.
Our approach involves working collaboratively with various partners to ensure effective support and positive outcomes. We connect people to community resources, build resilience, improve wellbeing, and coordinate social and clinical services around the client.
In short, we act as a link between clinical and non-clinical services, including other voluntary, community, faith, and social enterprise (VCFSE) services and housing, drug and alcohol services, and local education providers.
Our support is tailored to meet our clients’ cultural and social needs, aiming for sustainable positive outcomes. The key to our work is delivering coordinated, person-centred mental health support, ensuring people receive the right help at the right time to manage a wide range of needs.


We are so proud of the support all our staff give to the people in our community. Being able to hear the impact that this has on peoples’ lives is the best part of the work we do. The passion for helping people that everyone in our team holds is something to be proud of and celebrated.” – Robyn Butler, Open Mental Health Community Partnerships Manager
In addition to one-on-one support, our mental health locality team in Sedgemoor offers various group sessions and courses. Between May and September 2024, we held 69 group sessions, including anger management courses, mental health understanding courses, a women's ADHD support group, and regular coffee mornings.
Feedback from these courses has been positive. Participants have reported better understanding and management of anxiety and anger, improved mental health, and increased confidence. All participants who completed the feedback form noticed an improvement in their mental health since attending.
Dawn's story
When Dawn first met Claudia, she was struggling with the loss of her mum. She felt very anxious and was having panic attacks.
As her recovery and wellbeing worker, Claudia helped Dawn put in place the support she needed. She referred Dawn to bereavement counselling so she could start coming to terms with the death of her mum.
Dawn also confided that she was struggling to leave her house. As they talked, Claudia learnt that Dawn adored bird watching. So, Claudia suggested they visit a local nature and bird watching group together called Seeds of Hope.
They started gradually working towards going outside with the goal of building Dawn's confidence up so she could attend Seeds of Hope. At first, Claudia kept it as simple as opening the back door so Dawn could stand there in the doorway. Over time, Dawn could take one step outside, then two steps. Bit by bit she went further and further, and she began to look forward to her trips outside, and she realised things were worth living for.
The day Dawn and Claudia left the house to walk the three miles to Seeds of Hope was an amazing day.
Dawn says she will continue to go to the group on her own and is considering joining other groups including a coffee and chat group run by Second Step.


I was struggling with everything, day to day basics, going out… Just doing ordinary things…because of my anxiety and depression, because of the death of my mum. She was my life. I then got referred to Second Step. Claudia and me took steps by going out walking and getting me back in the open and helping me...
[It’s been like] going back to reality. I’ll be able to go out bird watching, which I couldn’t do, that’s another thing I want to start doing. I’ll be able to meet people, which I hope will help with my loneliness.” – Dawn
(Source: Bristol Wellbeing College data 2024)
Our colleges provide an extensive programme of free, interactive, psychoeducational workshops focusing on supporting people in their mental health and wellbeing recovery.
Sessions are written and developed in collaboration with people with their own experience of mental health difficulties. And through our sessions we share tools, skills, and strategies to help learners take control of their mental health and wellbeing.
Classes are delivered in community venues across Bristol and in Weston, Nailsea, Clevedon and Portishead in North Somerset. In August 2024 we began offering sessions in South Gloucestershire for the first time and these were very well received. We also offer online sessions and run Wellbeing Cafes in Bristol and North Somerset.
Analysis of Bristol Wellbeing College data showed significant improvements in learners' quality of life, social inclusion, psychological functioning, and mental wellbeing. North Somerset Wellbeing had an impressive 48% increase in attendance from the previous year with over 2,679 separate attendances. 70% of North Somerset learners completed evaluation forms with 90% giving positive feedback.
By building people's confidence, knowledge and skills, people reduce their reliance on other services now and in the long-term.

This group keeps me going – don’t think I’d be here if it wasn’t for the lovely group” – North Somerset learner
Higher Needs Floating Support
Higher Needs Floating Support in Bristol runs a number of services supporting people who are homeless or at the risk of homelessness. One of the projects is the Out of Hospital Service which was launched in October 2021.
It supports people who are at risk of homelessness following discharge from hospital. In total there have been 314 referrals to the service and 98% of clients did not return to rough sleeping due to the support provided.
Rachel's story
Rachel* has a history of self-neglect, trauma, and alcohol dependence. We met her following an emergency hospital admission where she was treated for severe abdominal pain. She had been told to leave her flat and had lost her bank card and phone.
We faced initial problems engaging with Rachel as she didn’t respond to calls or visits. In the end we gained access to her flat through a neighbour and discovered chaotic living conditions with old food, empty vodka bottles and an overwhelming smell.
We organised for Rachel to move out while the flat was deep-cleaned, made referrals to social care, bought her a mobile phone and food. We worked with her to put a care package in place to make sure she received regular support. And we saw immediate improvements in her health and wellbeing.
Rachel said:

I am forever grateful to my support worker Sophie and Ulla for their input following a hospital admission, as without it I believe I would potentially not be here today. I have struggled my entire life with my mental health and now with the right support, I am able to see things more clearly and a way forward out of the darkness. Thanks from the bottom of my heart.”
*not her real name
> Homelessness and complex needs services in Bristol and Somerset
Step Down in Somerset
Our Step Down service in Somerset, run by Second Step for Open Mental Health, supports people transitioning back into the community after a stay in psychiatric in-patient care. 95% of Step Down clients during 2024 have experienced homelessness.
The service runs daily from 9am to 5pm and provides practical living skills support, such as cooking, cleaning, and shopping. Additionally, it assists with budgeting, managing benefits, and making referrals to specialist support when needed.
Step Down adopts a trauma-informed approach, ensuring each client is treated as an individual with unique experiences and needs. Emotional support is also a key component, helping clients build confidence and resilience as they reconnect with their communities.
Step Down became part of the Open Mental Health alliance in June 2023, and is part of NHS Somerset’s transformation of mental health services, aiming to avoid hospital admissions by fostering strong community connections.
(Source: Step Down data reporting 2024)
> Homelessness and complex needs services in Bristol and Somerset
Link Team
The Link Team helps clients who are furthest from services, and who face multiple disadvantage, access the support they need. We do this by taking a multi-disciplinary approach to our work, trying to bridge the gaps between services.
The Link Team is a service for people who are street homeless, who experience severe emotional distress linked to a mental health problem and who face barriers accessing and engaging with support. Our main partners are AWP, St Mungo’s, Bristol City Council and Bristol Drug Project.
This year, we've experienced some amazing progress with our clients. The number of people who were street homeless has dropped significantly – from 81% at the start of their journey with Link to just 15% by the end of September 2024.
This change is huge and shows the power of our approach and that with the right support, people can really turn their lives around.
Building trust, staying engaged and responsive, and tackling different needs at the same time has really made a difference. We've also noticed the importance of supporting clients to get the mental health support they need, with an increase from 15% at the start of their time with us, to 46% of clients using mental health services in September 2024.
(Source: Link Team data 2024)
Bernie's story
Bernie* had a tough time living on the streets, struggling with both mental health and substance use issues. His situation was dire, with his mental health deteriorating and nowhere stable to stay. He ended up needing hospital treatment for his mental health after starting a fire in a park.
When the Link Team got involved, they took a proactive approach. They started building a relationship with Bernie while he was still in hospital, gaining his trust – for example, by accompanying him on day trips. This connection was crucial for Bernie to support a smooth transition back into the community. The team didn't just stop there; they also supported him in finding voluntary work and helped him navigate the complex housing system.
Despite the challenges, including pressure from hospital managers to discharge him quickly, the Link Team worked tirelessly to find Bernie a safe place to stay. Their efforts paid off, and Bernie eventually moved into his own home after a successful period in emergency accommodation.

The Link team's dedication and person-centred approach, based on My Team Around Me principles, made a significant difference in Bernie's life, helping him find stability and regain control over his future.
*Not his real name
> Homelessness and complex needs services in Bristol and Somerset
Step Together
Step Together works with people across Somerset who are homeless or at risk of homelessness, have complex needs and face multiple disadvantage. The service, which is commissioned by Somerset Council, uses a Psychological, Adversity, and Trauma (PAT)-informed model to help its clients discover meaningful and sustainable recovery.
Step Together has also been actively influencing change across services in Somerset; delivering trauma-informed training to housing and homelessness partners to help improve client experiences and outcomes across the county.
(Source: Step Together service data 2024)
An evaluation of integrating psychologists into a complex needs service like Step Together found that it improved the quality of the service, supported staff development and helped create change across the system.
A deep-dive listening exercise by Step Together’s client STAR group revealed that building trust and safety over time was particularly impactful for clients. Clients appreciated the understanding and support from recovery coaches, which helped them engage with services more effectively. One client said how Step Together never gave up on them.
In the 12 months leading up to September 2024, Step Together supported 197 clients with complex needs. In addition 78% of clients moved on from the service in a planned way, 95% of clients sustained their tenancies, 87% reported positive changes in mental health, 85% reported positive changes in drug and alcohol use, 93.5% reported positive changes in offending behaviours, and 89% reported positive changes in relationships.
John's story
One big issue facing many our clients is digital accessibility. Nowadays, accessing support, from applying for benefits to self-referring to services, often requires you to have access to a computer.
Our client John shared his insights into how isolating it can be if you don't have the kit or knowledge to make it work. He said, "I think it's tragic that you have to get to the position I was in to get help, because for lots of people that could be too late."
John has experienced homelessness, which negatively affected both his mental health and physical health. Because of his physical health issues, he needed accessible housing where he could live safely and comfortably.
However, he found not having an address and not having experience with computers were major barriers to accessing the support he needed:

Because I'm older, I'm 64, and I'm not computer literate. Some of the pressures that are on people of my age are about not being computer literate, and how your life can completely descend into complete chaos just because you don't know how to use a computer."
John started going to counselling, and was directed to Step Together. John found Step Together's help with the digital aspects of accessing support particularly helpful. Without Step Together's support, he says he could have easily ended up homeless again. "It's made all the difference," he told us, "not a bit of difference, all the difference. I can now think about how to go forward in my life, which I wouldn't be able to do if I was still homeless."
John now lives in his own bungalow which suits his accessibility needs. His goal is now to improve his social life as his new home is in an unfamiliar area where he doesn't know anyone – Step Together will be supporting him along the way.

John works well with people who can work with him on a deeper level. Working in a person-centred way really helped build the relationship between myself and John. I think John had been massively let down by other services and struggled after he had been belittled for being homeless." – Becci, John's Step Together recovery coach
> Homelessness and complex needs services in Bristol and Somerset
Changing Futures Bristol
Reducing the costs of supporting people facing multiple disadvantage
Here we look at the work of Changing Futures in Bristol. Changing Futures is part of a national programme looking at how best to support people facing multiple disadvantage in 15 areas across England.
What is multiple disadvantage?
The definition of multiple disadvantage, according to the Ministry of Housing, Communities and Local Government, involves people experiencing three or more of the following:
- Homelessness
- Substance misuse
- Mental ill-health
- Criminal justice involvement
- Domestic abuse

The challenges faced by people experiencing multiple disadvantage are often compounded by long-term experiences of poverty, trauma, abuse, and neglect. As a result, not only do people not receive the right support at the right time, but they often access services at the point of crisis which impacts negatively on both clients and staff teams, and hugely increases costs.
Recent studies estimate that not providing timely and effective support to people facing multiple disadvantage causes costs to increase by between £25k and £50k per person per year with an annual cost of £2 billion a year.
It is universally agreed that better coordinated and trauma informed statutory and voluntary sector approaches, like Changing Future’s My Team Around Me approach (see below) can reduce costs, support staff better and address inequity in the system.
Changing Futures’ focus has been to move away from crisis management towards building strong relationships with clients and professionals. In the first six months of the programme results show:
- The proportion of clients using A&E is down from 87% to 33%
- A significant reduction in homelessness applications
- The percentage of clients in temporary accommodation or sleeping rough down from 37.5% to 20%
My Team Around Me (MTAM)
My Team Around Me (MTAM) is a project run by Changing Futures Bristol aimed at helping people in Bristol who face multiple disadvantage.
MTAM brings together professionals from different services to help its clients to plan and remove barriers to recovery. Each of MTAM’s 54 clients is supported by at least three different services, and the Changing Futures service coordinators play a key role in facilitating collaboration between these services.
MTAM differs from typical multi-agency ways of working by bringing together professionals early to address each client's needs holistically. This approach ensures that clients receive continuous support and that the professionals involved share accountability.
Clients are encouraged to contribute to their plans, making the support more personalised and effective. The approach also considers clients’ cultural needs, ensuring that services are aware of and can work with the client's cultural background.
The programme has gained support from various sectors, including the NHS, criminal justice, and housing. Bristol City Council's MTAM approach strengthens this commitment further, leading to citywide improvements in collaboration and preventive safety planning.

I learned to be more accepting of other workers in the system and sort of try to put myself in their place, considering their response, such as does it come from a place of no capacity and burnout?" – MTAM Service Coordinator
Reducing out of area placements by 74%*
Formed in March 2022 under the umbrella of the Community Rehabilitation Service, Bristol’s Out of Area Placement Team supports people back into the community following lengthy mental health admissions. Many have been far away from their homes for years.
The work is part of a national initiative by the Government to end inappropriate out-of-area placements in mental health services for adults in acute inpatient care.
The team is a partnership between AWP, Second Step, and Bristol City Council, and works with people in high dependency rehabilitation units as far away as 170 miles from their homes, with an average admission length of nine years.
*Source: BNSSG Integrated Care Board
Reconnecting with life after hospital
Over the last two years the team has actively supported 14 people out of hospital and back into the community, continuing to work with them to help them settle into life outside hospital. Key to this support has been intensive engagement to build trusting relationships with clients and inpatient teams. Having a social worker within the team has bridged the gap between health and social care and helped smooth out the process.
A 2020 report by Rethink and the Royal College of Psychiatrists emphasises the negative impact of out-of-area placements, including higher costs and social dislocation. They advocate for reinvesting in locally provided services to improve outcomes and social participation for people with severe mental health conditions.
Shelby's story
Shelby had a challenging few years. At 16 years old, she was admitted to a mental health unit, and lived in various hospital wards being treated for complex Post Traumatic Stress Disorder (PTSD) and Borderline Personality Disorder (BPD) for 10 years.
Then she moved to Willow Ward, a Bridgwater-based mental health rehabilitation ward run by Somerset NHS Foundation Trust.
When she arrived at Willow Ward, Shelby hadn’t been outside alone for a year. As part of the Open Mental Health rehabilitation programme, she started working on getting her confidence back. Shelby said:

Willow was so good – I hadn’t been out on my own for over a year. They build it up slowly start with five minutes, then 10 minutes, 15, then half an hour. I was terrified about going out on my own, simple things like crossing the road I hadn’t done on my own for over a year. Willow helped get my confidence back."
Shelby also started working with Fran, a Rehabilitation and Wellbeing Worker from the Mental Health Community Rehabilitation Service. After getting to know Shelby, Fran realised she used to love to go horse riding, and this may be something she would like to try again.
Fran introduced Shelby to a local stables and they started to go every Wednesday afternoon. At first, Shelby wouldn't leave Fran's side and found it hard to speak to anyone. But over time, she became more confident and started interacting with and riding the horses.
"I find horse riding really therapeutic," Shelby said, "A horse called Maverick was my favourite. I fell in love with him. We would take them out for 45 minutes on the road. I started going on Saturdays with my parents and went twice a week for a while."
Before long, Shelby was teaching others how to ride and was able to visit the stables with Fran.
With her new confidence, Shelby has been able to move out into supported accommodation closer to her parents' home. She's planning to join a local stables, but still goes back to visit everyone at her old Stables near Willow Ward, including Maverick.


It’s wonderful to see the relationship Shelby has with Fran, her rehabilitation and wellbeing worker, and with everyone at the stables. By receiving the support she needed to pursue her passion, she’s been able to turn her world around. Shelby’s story is inspiring and will give hope to many.” – Sarah Cox, Service Manager for Open Mental Health Services in Somerset
Shelby shares her story with the BBC
After learning about Shelby's inspiring story, BBC Somerset journalists, Ross and Ruth visited Shelby and Maverick to find out more. Watch Shelby share her story on BBC Points West below:
As we move into 2025 we want to:
- Ensure the sustainability of our services despite the dual challenge of squeezed finances and increasing demand
- Work with our clients, colleagues and partners to create new recovery-focused community mental health services in Bath, Swindon and Wiltshire
- Contribute our expertise and insight to support the government's preventative and community-focused NHS agenda
- Continue prioritising collaboration and partnership as the best way to deliver outcomes for the people who use our services.
If you are interested in talking to us about what we do including our trauma-informed training and consultation work, please do get in touch!
Contact Jane Edmonds, PR & Communications Manager:
If you are interested in finding out more about our work or getting involved, please contact:
Alice Peycke, Head of New Business:
Our services
We provide mental health and support in Bath and North East Somerset, Bristol, North Somerset, South Gloucestershire and Somerset. Click the following links to find out more about our services, projects and partnerships: